A hiatal hernia can be diagnosed with a specialized X-ray study that allows visualization of the esophagus (barium swallow) or with endoscopy. Paraesophageal hernias are best diagnosed with a barium swallow, although their presence is usually suggested by endoscopy that is being performed routinely for unrelated symptoms. In instances of paraesophageal hernia involving organs other than just the stomach, a definitive diagnosis is established with CT or MRI.
Preoperative testing will usually encompass esophageal manometry for evaluation of esophageal motility disorders, measurement of esophageal body peristalsis as well as measurement of the lower esophageal sphincter position, length, and pressures.
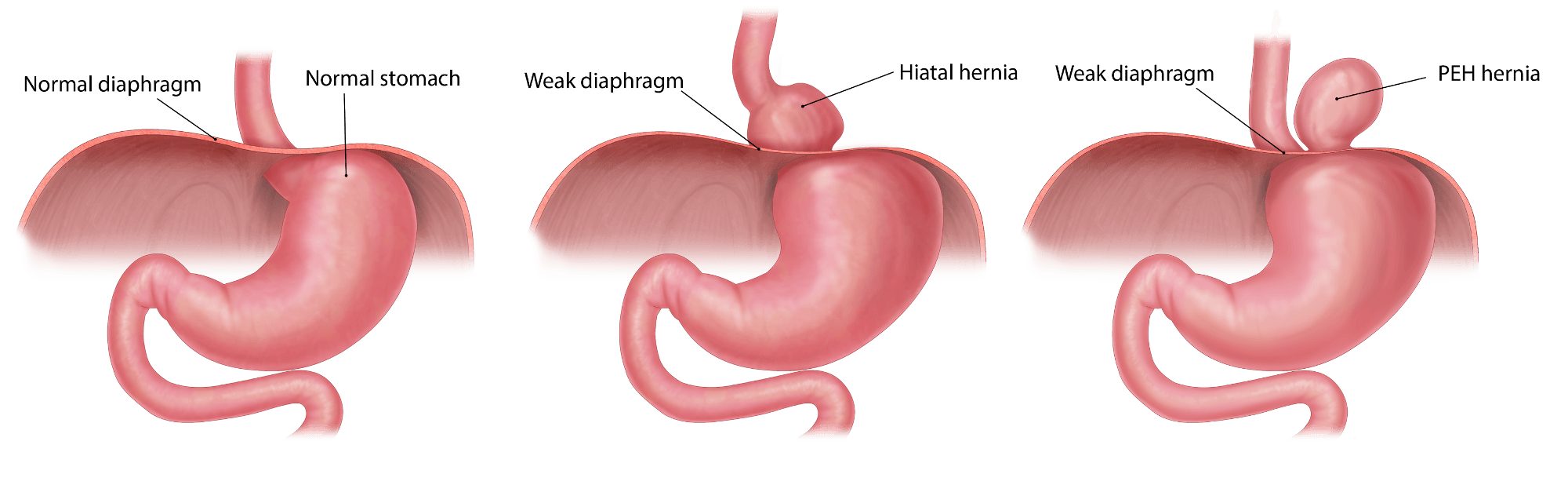
A paraesophageal hernia is treated surgically and a true paraesophageal hernia is considered a surgical urgency. It carries the risk of stomach volvulus (twisting of the stomach), which can cause total obstruction of the stomach, and if persists, stomach perforation and generalized severe abdominal infection (peritonitis).
The surgery can be done laparoscopically with small incisions. Even at times if a recurrent hernia is present, it is best approached laparoscopically. At GBMC, Dr. Ahmad Bashir has a great experience with these procedures, initial or recurrent.
The procedure may entail the use of mesh to close the hernia defect itself, especially if it is large and tension may be present on weak diaphragmatic muscle tissue if closed without mesh. If symptoms of reflux are present, then a fundoplication is also done (wrapping the stomach around the esophagus) to treat reflux at the same time. If not, at least Gastropexy (fixing the stomach to the abdominal wall) is done to minimize the risk of recurrence

