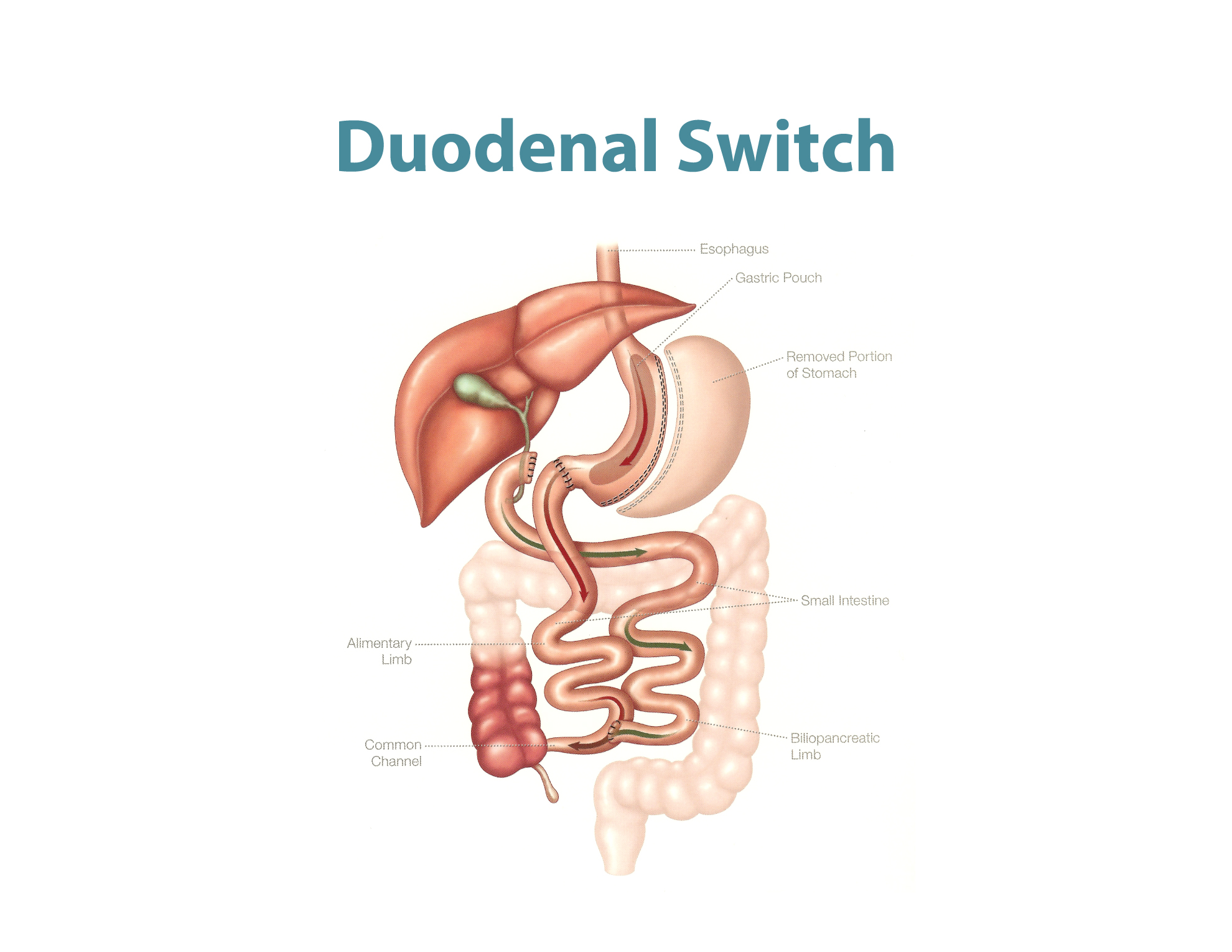
The Duodenal Switch (DS) operation was first reported by Dr. Hess in 1986. It is a variant of another operation called Biliopancreatic Diversion (BPD) invented by Dr. Scopinaro. The main advantage of this procedure is the higher rate of weight loss, and it is definitely sustained longer compared to all the other procedures. It also carries a higher remission rate from Diabetes compared to all other procedures. Remission rates for early Diabetes approach 100%, while even for late Diabetes or high Insulin requiring patients can obtain above 80% remission rates as opposed to 55% in gastric bypass. As in the picture above, it has two components:
A Vertical Sleeve of the stomach:
Cutting the stomach vertically into a sleeve, decreasing the amount of food intake more than BPD, but definitely less than gastric bypass patients. The first portion of duodenum, which is tolerant to all gastric acid, is preserved and this decreases the incidence of ulcers compared to BPD and Bypass patietns. It also increases protein absorption compared to BPD, causing less protein calorie malnutrition.
Bypass of 50% or greater of the small intestine:
Bypassing the majority of intestines and preserving only 75-100 cm of intestine for absorption just like the BPD operation. However, there are other variants and modifications to the length of the intestine bypassed to decrease the malabsorption issues. In our center, we preserve a common channel of at least 100 cm or 10% of the entire small bowel length if more than 10 meters, with an additional 30% (around 250-300 cm) Roux limb (can still absorb certain elements of food) for the same total alimentary limb described as the original surgery (at least 350-400 cm alimentary limb length). This would minimize the malabsorption of vitamins, especially fat soluble ones (A, D, E, K), as well as other food elements, and decreases the incidence of diarrhea and foul smelling stools. It is still a risk however, with this procedure compared to standard proximal gastric bypass. In certain cases however, we utilize only 100 cm of common channel with 150 cm Roux, for a total of 250 cm only, when severe obesity is present despite a previous bariatric procedure.
Overall the modified version provides less malabsorptive complications, more sustained weight loss, and more food tolerance. It still provides better Diabetes remission rates compared to the gastric bypass, especially for those who have long standing Diabetes, or on high insulin requirements. It also does not carry the risk of marginal ulcers as in BPD and gastric bypass patients from acid, smoking or NSAIDs use. Its single anastomosis version (SADIs) is simpler and quicker, and is carried as the first option here at our center for some patients, as a primary procedure.
However, it does not provide the benefits of treating Gastro-Esophageal Reflux Disease (GERD), which would still be a problem for some patients. It also does not limit sweet intake by patients as the gastric bypass operation does, which can be a problem for sweet eating patients.
The incidence of complications in the modified version is less than the original one, but slightly higher than the gastric bypass. It does need more stringent follow up, especially for vitamin levels. The potential complications are:
- Leak: incidence is 1-2%.
- Diarrhea & Foul smelling stools: (less with the modified version). Potential incidence increases with more carbohydrate & fatty food intake.
- Reflux disease in around 20% of patients as stomach still retains its acid production ability.
- Vitamin deficiencies in 25-30% of patients: usually with the original version more than modified one. But it still poses a more significant problem definitely with non-compliant patients.
- Internal hernia rate 1-2%: similar to the gastric bypass.
- Protein-Calorie malnutrition: less than BPD, and definitely less with the modified version.

