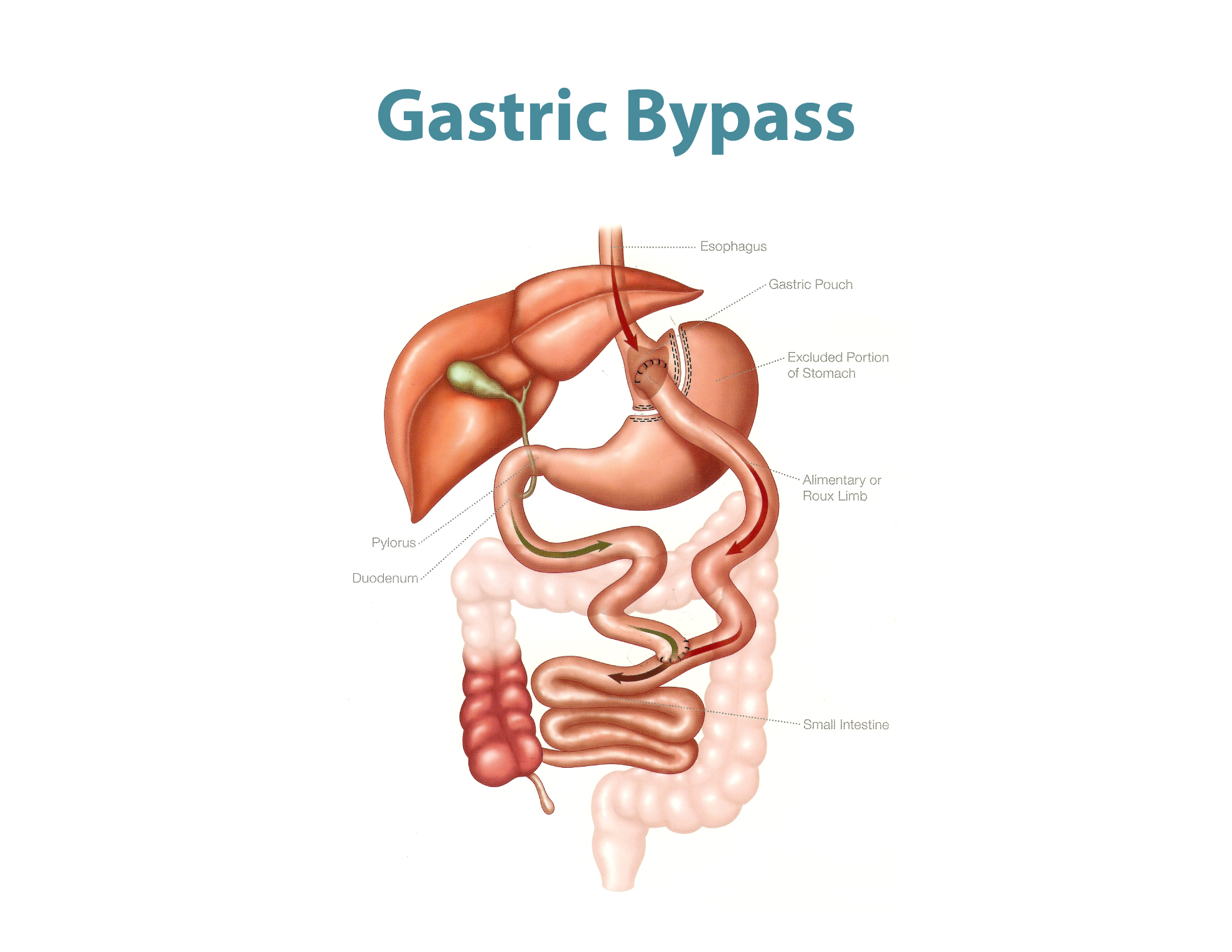
This operation is considered the mother of all, and oldest. It has been done since 1960s by the father of Bariatric Surgery Dr. Mason. However, it continued to evolve overtime to what it has become over the last 20 years. It entails creating a new small 15 cc stomach, and bypassing the rest of the stomach, initial 3 feet of small intestine, while performing two connections between the new stomach and small intestine, and the second between small intestine and small intestine, as shown in the picture. This is called the “Proximal” Gastric Bypass, which causes a variety of changes in the gut environment, including its hormones, without causing significant malabsorption. The normal length of intestine is 20-25 feet, so a patient still has additional 17-22 feet to absorb all nutrients necessary.
Having said the above, the patient’s average daily caloric intake after LRYGB is 800-900 Kcal per day. Hence, it is of utmost importance to prioritize what a patient eats: Protein first, Vegetables and Fruits second. Carbohydrates should be the least significant absent part of your diet. The patient will experience what we call “Dumping Syndrome”: feeling dizzy, light headed, heart racing, crampy pain, and diarrhea if she/he eats a high sugar load, thus the added benefit if sweets are the main contributor to the patient’s obesity.
The patient should expect to lose 60-80% of her/his excess weight. Weight loss initially is rapid and spontaneous. The patient should exercise to maximize the weight loss, as well as to preserve her/his muscle mass while losing the fat mass.
The most exciting part about this procedure is that it established surgery as a treatment and a chance for cure from Type II Diabetes. A patient with diabetes and obesity, has > 80% chance for resolution of (remission from) Diabetes after this procedure. This is independent from weight loss, as it almost happens immediately after the procedure, unlike other surgical options. Resolution of other associated medical problems are also higher.
The immediate complications from this procedure are slightly higher compared to others. The most serious occur in 1-2%.
They are related to technical issues immediately at the time of surgery:
- Leak: from connections or staple line failure occurs in <0.2% at GBMC, this requires an immediate operation for the repair of the leak, laparoscopically most commonly.
- Bleeding: requiring return to the operating room or blood transfusion in 1.7% of procedures.
Other late early complications:
- Stenosis of the upper connection (Gastrojejunal anastomosis): narrowing by overhealing of the upper connection occurs in 1.9% of patients. Patient experiences difficulty keeping food down with no pain. This usually happens around 3-5 weeks after surgery. This narrowing can be dilated with simple outpatient endoscopy, not surgery.
As for the chronic complications:
- Marginal ulcer: ulcer at the top connection, occurs due to either smoking or taking anti-inflammatory pain-killers (NSAIDs) like, Aspirin, Mortin, Brufen, Volatrin, Diclogesic, Alleve, Advil or Naprosen. The treatment is avoiding the cause and a simple acid reducing pill (PPIs).
- Internal hernia with risk of intestinal obstruction: in < 2% of patients. Patients usually experience abdominal pain, bloating, relieved after diarrhea. It usually occurs in episodes. This is confirmed at times by a CT scan. Treatment entails a surgical procedure that can be laparoscopic most of the time, with closure of the hernia defect.
Long-term follow up is also important to ensure patients proper nutritional status. Lab tests are done at least annually, or as necessary to check the level of different vitamins and minerals. With regular follow up, the patient should achieve his goal in 90-95% of the time, as this procedure has a low rate of weight regain.

